Healthcare fraud in the United States takes billions of dollars from patient care resources annually, making hospital management and finances more challenging. Manual inspection methods and fundamental statistical data analysis in fraud detection systems deliver unreliable outcomes that take too long and cost too much money. We need a better and faster way to address these problems.
NLP offers a groundbreaking modern approach to finding and stopping healthcare fraud. With sophisticated algorithms, NLP examines detailed data collections to detect hidden trends and report suspicious findings. Its versatile data processing system examines fixed information alongside irregular patterns to detect fraud patterns that escape other detection methods. Healthcare systems can now rely on NLP to spot new types of fraud early through advanced analytic methods.
How can NLP enhance Healthcare Fraud Detection?
1. Key Data Sources for Fraud Detection
To detect and prevent fraudulent activities, NLP utilizes various data sources:
Claims Data
Insurance claims provide crucial details about doctors' diagnoses, medical procedures patients receive, prescription information, and bills paid. NLP algorithms read through the data and detect abnormal findings.
Clinical Notes and Reports
Healthcare providers create many health records, from their medical notes to discharge paperwork and lab reports. NLP searches for essential data elements to locate suspect patterns or strange activities.
Patient Demographics and Medical History
NLP analyzes patient personal data, medical history, and insurance records to find signs of healthcare fraud.
Social Media and Online Activity
NLP checks what patients share on social media platforms to find unusual or wrong patterns.
NLP achieves better fraud detection results by uniting information from different data sources to form a complete perspective.
2. Advanced NLP Techniques for Fraud Management
NLP employs a range of sophisticated techniques to uncover fraud:
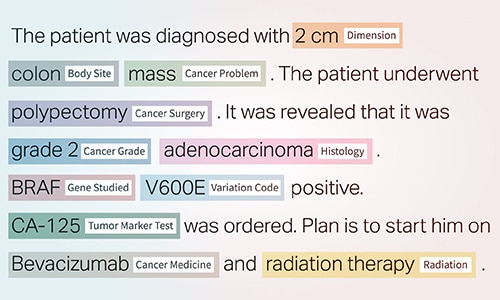
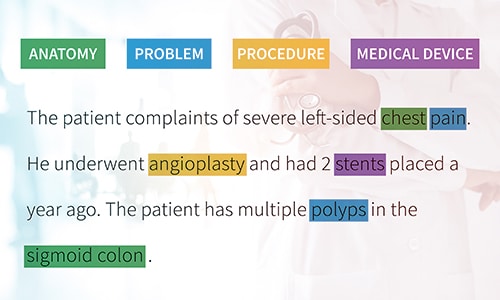
Named Entity Recognition (NER)
The NER system extracts essential health information from free-text medical documents to create a structured database.
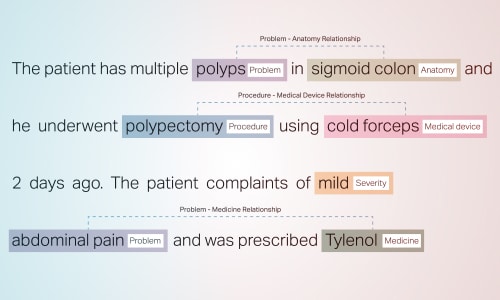
Relationship Extraction (RE)
This system finds links between healthcare data points by showing how patients connect to providers and what medical treatments match specific diagnoses.
Text Classification
Machine learning systems identify fraudulent claims by recognizing unusual data behavior.
These techniques enable real-time detection of complex fraud patterns, significantly enhancing efficiency compared to traditional methods.
3. Common Fraud Scenarios Addressed by NLP
NLP is particularly effective in identifying the following types of healthcare fraud:
- Upcoding: Staff bills insurance companies for more costly treatments than they performed.
- Unbundling: Including separate fees for medical services that need to be combined into one listed service item.
- Duplicate Billing: Submitting multiple claims for the same service.
- Phantom Billing: Filing paperwork to collect payment for nonexistent treatments.
- Prescription Fraud: Our system studies how doctors prescribe medicine to identify abuse of drugs, problematic prescribing trends, or unauthorized distribution of medications.
Thanks to the healthcare NLP, which automatically detects different types of fraud, healthcare organizations can save money and maintain trustworthy business practices.
Benefits of NLP in Healthcare Fraud Detection
Integrating NLP for fraud detection delivers several critical benefits:
Enhanced Accuracy
NLP's automated technology detects fraud more accurately in extensive data collection than people do.
Cost Efficiency
Checking for fraud as soon as possible helps protect against wasted money in fraudulent cases.
Time Savings
Automating fraud detection helps medical staff allocate their time better by reducing their burden while ensuring quality patient care.
Proactive Risk Management
Our system tracks real-time data so staff can immediately stop fraud attempts.
Data-Driven Insights
NLP identifies meaningful patterns to help healthcare leaders make better fraud prevention and operation plans.
Additionally, NLP helps reduce manual errors by offering higher fraud detection reliability while continuously improving its predictive capabilities. This continuous learning process allows organizations to stay ahead of emerging fraud tactics and adapt swiftly to new fraud trends.
Implementation Challenges
Despite its potential, adopting NLP for fraud detection involves several challenges:
- Data Quality and Availability: NLP needs highly formatted and complete datasets to work well. Poor data quality can lead to inaccurate results.
- Model Development and Optimization: Developing and improving NLP models requires skilled experts and additional resources, such as processing power.
- System Integration: NLP tools face significant difficulties when developers try to connect them to existing healthcare systems.
- Ethical Concerns: Security and privacy measures for handling confidential health data come first in our priorities.
To achieve optimal fraud detection through NLP, we must tackle these problems first.
Future Trends in NLP for Healthcare Fraud Detection
Advancements in technology and innovative applications shape the future of NLP for healthcare fraud detection:
- Advanced NLP Models: The latest NLP systems, BERT and GPT, successfully analyze written documents and text. The models track strong hidden connections to spot multilayered fraud activities, including manipulating codes and claim fraud.
- Integration with Healthcare IT Systems: EHR integration enables health facilities to receive all medical information in one system. Access to claims and healthcare records lets us track and prevent real-time fraud.
- Practical Implementations: Optum applies NLP technology to solve actual problems by identifying duplicate billing and prescription fraud for real-life use.
- AI and Machine Learning Synergy: By connecting NLP with AI and machine learning systems, detection models will become better at adapting and predicting fraud. Healthcare organizations can predict fraud risks better by constantly monitoring their real-time data.
Medical facilities will integrate updated natural language processing systems into their fraud monitoring platforms to reduce risk more effectively.
Final: Securing Healthcare’s Future with NLP!
Natural Language Processing (NLP) has unique abilities to solve healthcare fraud problems and risk management needs. Healthcare NLP protects organizations by searching massive amounts of data for suspicious activities, which helps reduce expenses and make operations more effective.
Our success in today’s evolving industry depends on fixing the key problems: clean data paired with seamless systems and strict privacy rules. The growth of technology will allow Natural Language Processing systems to protect healthcare data and keep information reliable.





